Climate change involves two major types of change. First, there is overall progressive warming. Second, there is increased variability/unpredictability in weather patterns. Both types of change impact negatively upon human respiratory health. Worsening air quality and increased allergens can worsen existing disease. Climate-related changes in allergens and in vectors for infection can cause new disease. Redundant sophisticated studies have projected marked increases in respiratory morbidity and mortality throughout the world as a direct result of climate change.
Changes in climate constitute a reality that, according to recent projections, is going to worsen in the coming years. Climate change represents a massive threat to respiratory health: 1) by directly promoting or aggravating respiratory diseases; or 2) by increasing exposure to risk factors for respiratory diseases. Climate change increases the amount of pollen and allergen produced by each plant, mould proliferation and the concentrations of outdoor ozone and particulate matter at ground level. The main diseases of concern are asthma, rhinosinusitis, chronic obstructive pulmonary disease (COPD) and respiratory tract infections. Groups at higher risk of climate change effects include individuals with pre-existing cardiopulmonary diseases or disadvantaged individuals. Adaptation and mitigation measures are strongly needed.
It is now widely accepted that the earth’s temperature is increasing, as confirmed by warming of the oceans, rising sea levels, glaciers melting, sea ice retreating in the Arctic and diminished snow cover in the Northern Hemisphere. Moreover, changes are also occurring in the amount, intensity, frequency and type of precipitation, as well as the increase of extreme weather events, such as heat waves, droughts, floods and hurricanes [1–3]. Most of the observed increase in globally averaged temperatures since the mid-20th century is probably due to the observed increase in anthropogenic greenhouse gas (namely carbon dioxide, methane and the nitrous oxides) concentrations [1]. Projections of future greenhouse gas emissions indicate a worsening of the situation with between a 1.1 and 6.4°C increase in the mean temperature by the end of the 21st century [1].
Climate change represents a massive direct threat to respiratory health by promoting or aggravating respiratory diseases or indirectly by increasing exposure to risk factors for respiratory diseases [4]. Climate affects weather, air and water quality, local and national food supplies, economics and many other critical health determinants. Observational evidence indicates that regional changes in climate, particularly temperature increases, affect a diverse set of physical and biological systems in many parts of the world [1, 2], some of which are of concern for respiratory health.
A body of evidence suggests that major changes involving the atmosphere and climate have an impact on the biosphere and human environment. Increased concentrations of greenhouse gases, especially carbon dioxide, in the earth’s atmosphere have already substantially warmed the planet, causing more severe and prolonged heat waves, temperature variability, increased length and severity of the pollen season, air pollution, forest fires, droughts, and heavy precipitation events and floods, all of which put respiratory health at risk [4]. A synthesis of respiratory health effects due to climate change is presented in figure 1. The main diseases of concern are asthma, rhinosinusitis, COPD and respiratory tract infections, but the extent to which these are spread will vary according to the proportion of susceptible individuals in a given population.
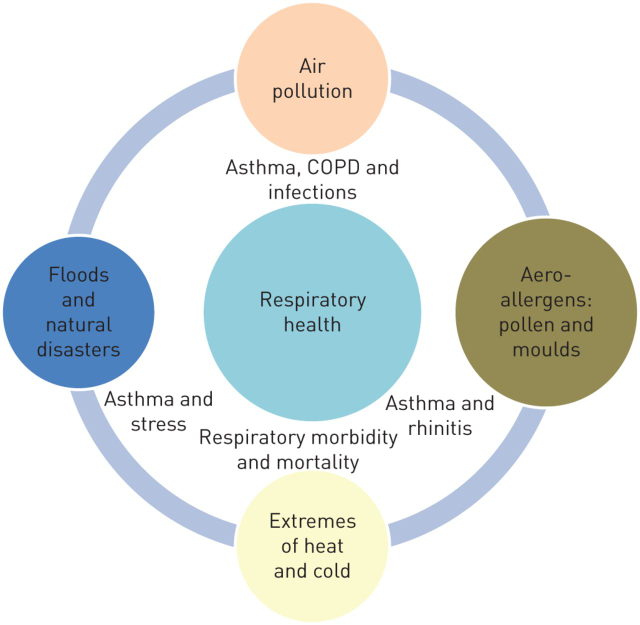
Figure 1. Potential respiratory health effects of climate change. COPD: chronic obstructive pulmonary disease. (https://err.ersjournals.com/content/23/132/161.full#xref-ref-4-1)
Individuals with pre-existing cardiopulmonary diseases are at higher risk of suffering from climate changes. Areas of greater poverty with limited access to medical care will suffer more, as will areas with less well-developed medical services, which are likely to include disadvantaged groups, migrating populations and areas with the greatest population growth [5].
Climate changes affect many physical and biological systems, including the immunological and respiratory systems that are critical to human health, and it is foreseeable that environmental risk factors will have a stronger effect in the coming years. To summarise, chemical air pollutants and anthropogenic aerosols can alter the impact of allergenic pollen species via two mechanisms. First, physical, chemical and biological interactions can change the amount and/or features of the allergens in the air, for example, via chemical stress of plants, protein nitration and pollen breakup with allergen release. Secondly, the susceptibility of humans to allergens can increase in the presence of chemicals and aerosols, e.g. diesel exhausts, ozone and nitrogen dioxide, as well as particulate matter. Climate changes interact with and affect air pollution and pollinosis, which in turn increases the frequency and severity of asthma and affects the clinical expression of allergic disease. Climate change affects the timing, dispersion, quantity and quality of aeroallergens and the distribution and severity of allergic disease. Climate change alters local weather patterns including minimum and maximum temperature, rain precipitation and storms, all of which affect the burden of allergic disease. A combined approach comprises primary prevention by greenhouse gas mitigation to stabilise the climate, and secondary prevention by clinical intervention to minimise climate change-related increases in asthma and allergic disease. Climate changes in the future may depend on how rapidly and successfully global mitigation and adaptation strategies are deployed. The effect of human intervention and efforts to minimise changes in vegetation and aeroallergen exposure remains to be seen [5].
Increases in air and water pollution due to climate change are at the origin of both respiratory infections and aggravation of chronic respiratory diseases, such as asthma and COPD. The extent to which air pollution is also responsible for the development of such complex diseases is still under debate. Overall, reducing air pollution might contribute to lessening of the impact of climate change on patients [5].
What can we do to decrease the effects of environmental factors affecting respiratory diseases? Suggested measures are as follows: 1) encouraging policies to promote access to nonpolluting sources of energy; 2) reducing the private traffic in towns and improving public transport; 3) decreasing the use of fossil fuels and controlling vehicle emissions; 4) planting nonallergenic trees in cities, and in this context the proposed plantation of new trees should be evaluated by allergy specialists in order to avoid high allergenic species. Many measures to reduce greenhouse gas emissions may have positive benefits for health. These co-benefits will offset at least some of the costs of climate change mitigation and should be taken into account in international negotiations. Strategies to reduce climatic changes and chemical and biological air pollution are political in nature, but citizens, in particular health professionals and societies, must raise their voices in the decision process to give strong support for clean air policies at both national and international levels. The increased risk population have to be especially addressed.
References
This website was produced with the support of the United States Agency for International Development (USAID) under the terms of USAID's Research for Decision Makers (RDM) Activity cooperative agreement no. AID-388-A-17-00006
Views expressed herein do not necessarily reflect the views of the U.S. Government or USAID. icddr,b is also grateful to the Governments of Bangladesh, Canada, Sweden and the UK for providing unrestricted/institutional support
68, Shaheed Tajuddin Ahmed Sarani Mohakhali, Dhaka 1212, Bangladesh
icddr,b is located at the Mohakhali area in Dhaka, just ask your driver for the "Cholera Hospital"
